This year has seen some good news in the market for health insurance, with relatively low inflation in rates.
Competition in the market, and new techniques to help employees stay healthy are among the factors holding costs.
But even though the growth in health care costs has slowed, it still may be rising at an unsustainable pace. And insurers, providers and employers will be challenged to bring expense growth down further. High-priced, lifesaving drugs and a shortage of physicians are among the challenges.
We assembled a panel of experts to discuss the market at our Trends & Innovations in Health Benefits & Care event last week at the Arden Hills Country Club.

What follows is a transcript of our discussion, edited for length and clarity.
Steinhauer: Let’s talk about trends in the cost of care. Covered California, in the individual market, recently said it expects a rise in insurance rates of less than 1% going into next year. Renee, maybe you can start us with this: What are you seeing with your clients in terms of the trend in inflation in insurance rates?
Bosley: There’s two things to consider: One is the cost of the insurance to cover the care, and the second is the cost of the care itself. Medical inflation in July was 2.9%, down from a long-term trend of 5.8%.
One of the things that’s driving costs down is the actual better organization around care.
But the other factor really is the pool, the block of business. If you think about the individual market, when we first set up the exchanges, underwriters had to predict the cost needed to make sure that there were enough premiums to offset claims, right? We didn’t know how many people would enroll. There was a lot of uncertainty. In my opinion, the individual market now is stabilizing. It’s become more predictable.
On the employers’ side, it’s really different. It depends on the size of the group. It depends on whether they’re in a pool or are they rated on their own and how they’re performing. This can cause a lot of confusion because I’ll have a group with Blue Shield get a 12.9% increase. That’s their trend for Q1. And they’ll say, well how come (another group) got a decrease with Blue Shield? Well, larger employer, different population, they’re not in that pool.
In the group space, the carrier will look at their block of business in that pool, see how it’s performing and just like in the individual market space, they’ll try to predict where they think they need those increases to go. They’ll start with medical inflation, they’ll start with other risk factors and they’ll have to project forward.
It’s interesting to me that the individual market has become more stable at this point and is trending better than the group market, in my opinion, in that pooled space.
Steinhauer: William, what are you seeing in terms of the trend in the cost of health insurance for both Sutter Aetna’s clients and from your competitors?
Huff: We are certainly seeing the similar moderation in costs. If you look at what the National Business Group on Health recently said in their 2019 survey, those employers are seeing about a 6% cost trend. We’re seeing similar single-digit cost trends.
Employers now understand the importance of being able to attract and retain employees in this very-low-unemployment market. They also understand the importance of the right benefit package. That also means they’ve got to keep that benefit package structured in a way to moderate those costs over time.
What that has meant is that they’re looking for opportunities to understand where they can partner with health systems like Sutter Health Aetna. One of the particular things that we’re doing is making sure that those employees can engage early on into the health system. Much like the banking industry now wants to push out technology to all of our pocket computers, our iPhones and other devices, that’s what we’re seeing as one of the main techniques to help moderate costs. It’s to get those employees anytime, anywhere access to their health care systems.
We’re all now in a world of time shifting, right? We’re DVRing shows, watching them when we want. Health care’s really developing that way as well, where with own mobile devices, when there’s a health need, we’ve got telemedicine capabilities that are able to meet the need. That then keeps both facility costs and cost of care down.
The other big trend is that those of us in health care know that it’s really 20% of the population that’s really driving 80% of the cost. We all understand that we’ve got to get the congestive heart failures, the diabetes, hypertension, we’ve got to get those things under control.
The good news is that we understand that we’ve got to address the entire person. That includes the behavioral health aspect that is so important. We can’t get a diabetic to test his or her own blood sugar if they’re in a mentally unstable state, whatever that might be.
Being able to see the patient holistically, those are the kinds of things that are going to keep (costs) moderated.
Field: The numbers that I’ve seen agree that we’re in a lull in that hyperinflation that we were experiencing three or four years ago. I just read a story of a woman who came to the emergency department frequently for her asthma attacks. It was costing the insurance company a lot of money. But through this holistic approach where they focused on the patient instead of just saying, hell that’s their problem, the doctor authorized a cleaning crew to go to the patient’s house and get all the dust up. That actually reduced the frequency of emergency visits. In the old days that would not have worked out. There was no way for one pocket to pay for this other thing. But when we bring all of that under one medical home, then these outreaches make more sense.
So I do see some movements that are mitigating the increases. But I see some dark clouds on the horizon that threaten the stability of the system.
Steinhauer: Back to Renee: In terms of other costs of health care that are not captured within insurance coverage, things like copayments and drug costs, what are you seeing in terms of the industry making progress and holding those down?
Bosley: (The U.S. Department of Health and Human Services) is asking for an end to surprise billing. When you go in and have a knee replacement done, you pay for the surgical center, the anesthesiologist, the surgeon, and you’ve done your work looking for an in-network provider and facility. But who’s in the room? A physician’s assistant who’s an independent contractor and he’s out of network. So you receive all these different bills, especially if you’re in a (health savings account) where you’re going to pay initially. You can’t figure out what you owe and how does an out-of-network person sneak in there, and why do I owe more? So it’s a problem.
One of the things that I’m excited about is a company, there’s a number of them, but one of them is called PriceMDs. They have negotiated bundled pricing for hips, knees, shoulders, expensive imaging through 1,400 surgical centers and 4,100 imaging centers. I have a client right now who’s actually giving a cash bonus to employees who use the facility in the PriceMD network because it’s a flat price. It’s one bill for everything. Why can’t we do more of that? That’s what excites me.
Field: There are a lot of other things that will work to bring the cost of medicine down. I believe that the way the curve will be bent is by expanding the pool of prescribers. Psychologists, pharmacists, physician assistants and nurse practitioners will be granted prescribing privilege. The trend has already begun throughout the country. It’s more advanced in some states and less advanced in others. This is what’s going to dramatically bring down the cost of medicine because when you open up the pool of prescribers, then you can bring real price controls or competition into the situation.
Steinhauer: Renee, with all of these efforts to control cost, what is happening with the quality of care in your view and your clients’ observation? Is it improving or degrading?
Bosley: One of the things that’s leading to better quality of care is getting involved sooner, steering that employee, engaging them. And then the employer now has the opportunity to incent that. We go to their mobile app and say, “It’s time to get your (blood sugar) checked. Make an appointment now, you can have $100 towards your wellness program.” We’re hoping that we can change behavior that way.
I’m going to add one more quick note: I was in the boardroom with a client in Arizona recently and the owner said, “Renee, if I have a diabetic who’s not getting their blood glucose checked and we’ve removed all the barriers and they’re not willing to engage in doing anything about it, can we charge them more?” That’s an interesting conversation.
So employers are looking not just at premiums and benefits, they’re looking at their population risks. They’re looking at the 20% that’s driving 80% of the costs, and they’re talking about sticks and carrots and it’s just driving new conversations with employers.
Now that we’ve got this data, now that we can see the risk and we can see who’s engaging and who isn’t, I’m excited about the fact that we’ve got that information. It’ll be interesting to see how many employers choose to motivate with incentives or maybe even charge more for members who aren’t engaging. That might be a way to start changing that behavior and steering them where we want them to go.
Steinhauer: Can the employer charge them more?
Bosley: Yes. You have to follow certain policies, (but) so as long as you’re compliant, yes, you can do it.
Steinhauer: Will, what’s your observation about the quality of care and the direction it’s going?
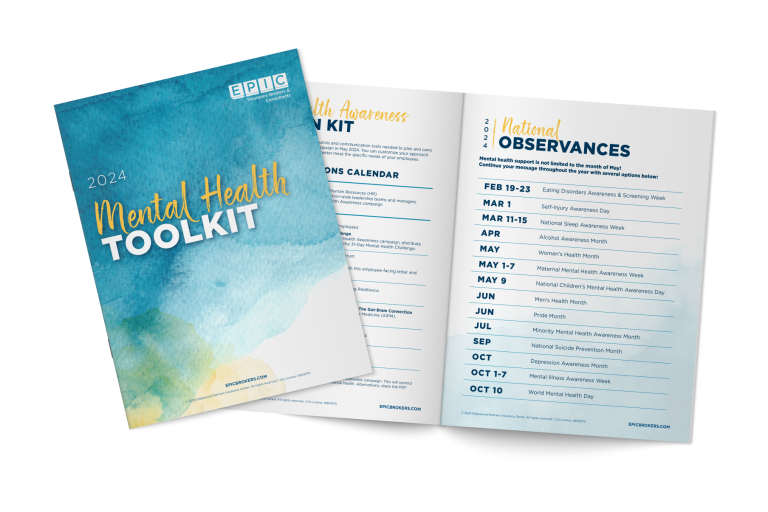
Huff: I’m a data guy. From a data perspective, it’s really about if you can’t measure it, you can’t improve it. Large, Fortune 500 companies will often have an epidemiologist on staff. And (insurance consultants) are actually driving that level of data measurement and quality measurement into mid-size and smaller-tier employers. Firms like Epic can come in and explain to them the actionable initiatives that you can take to drive quality to put into programs. Turn the data into information that becomes actionable. Then we will drive behaviors both at the individual level and then at the plan sponsor level.
Steinhauer: I’m going to ask about how health care has been in the news lately. Some of the Democratic presidential candidates have been discussing Medicare for All and the possibility of Medicare for All even without private health insurance. What would this mean for employers and their employees’ health coverage?
Huff: Well, let me be very clear: As a private citizen, I do not speak for Larry Merlo, (CEO of Aetna parent company CVS Health), nor Sarah Krevans, (CEO of Sutter Health). Having said that, the key point is what does Medicare for All really mean? At this point, it’s really all about the politics and the optics. We know that Medicare is a very popular program. It’s being used, quite honestly, just as a marketing technique.
Now, having said that, what’s also clear is that in the marketplace, the seeds of the Affordable Care Act are still germinating. There are now more plans who plan to enter the market on the Affordable Care Act (exchanges) than have canceled. That’s what we really need. So I just say let the market take place with some government incentives. We’ve seen the proof in the pudding of how that can work out.
Field: I think that there’s a couple of truisms that I’d like to put out in front before answering the questions. One, when you have unlimited coverage, you’re going to have unlimited need. So when you say we’re covering everybody for everything, the amount of need will increase astronomically beyond what is projected. Almost the flip side of that is coverage does not equal care. We can provide all the “coverage”— get out those air quotes — we want, but that won’t translate to care because there are not enough caregivers. There are not enough doctors out there to deliver the care as (the health care market is) currently structured, which is why I believe that we will see this expansion of prescribing into the other professions. It’s one of the things that will address that.
Steinhauer: What could the continued legal attacks on the ACA mean for employer-sponsored coverage?
Field: I think the current paradigm is untenable. I don’t see how we can continue to promise unlimited care for an unlimited number of people. Some of the candidates are talking about insuring non-citizens. If you say we offer unlimited care here to anybody who’s inside our borders, what will happen to the transfer of people who desire that care? Do we not see Canadians coming across the border for hips, just like we do see Americans buying Canadian drugs to get a reduction? The money will talk in that regard. I see that breaking down.
I think we’re going to end up with a two-tier system. We’re talking not in the next five years. But we will have a two-tier system in which the government will mandate a basic level of care. It will not be provided directly by physicians. It’ll be provided by a team, of which maybe a physician will be the head of. Who knows? And then there’ll be a supplemental market, which is where Aetna and Blue Cross and so forth will be able to compete. The employers, I think, are going to want to be able to offer this as an incentive in a tight (labor) marketplace.
There are trends that are really heavily impacting this. I’m not sure if anybody is familiar with the impact of specialty drugs, but these are drugs with an astounding price tag. The one that I was just focusing on is Zolgensma: literally $2.1 million for a single treatment. These drugs are used to treat perhaps 1% of your workforce, and they cost between 30 and 50% of your drug expenditures. That trend is going to break the bank.
Related Content
Products
Employee Benefits Consulting
Our dedicated EPIC benefits team is focused on delivering better outcomes – to both your benefits program ...
Products
Wellbeing & Health Management
Our Wellbeing and Health Management consultants help you create a strategy around population health ...
Industries
Healthcare
Our healthcare practice is known around the world for its expertise and passion in delivering exceptional ...