Viewpoints from Sarah Fleming
Benefits leaders understand that the next generation of GLP-1 drugs is creating a need for improved management and strategic oversight. At times, the importance of these medicines in managing patients with diabetes can be lost with so much focus on their ability to achieve weight loss in patients for whom that once seemed impossible. Without question, both diabetes and obesity are chronic diseases that impact a large number of Americans.
- Diabetes affects 13% of the U.S. population, with healthcare costs totaling $413 billion.1
- Obesity is prevalent, with two out of five U.S. adults affected, leading to annual healthcare costs of $173 billion.2
- Various GLP-1 (glucagon-like peptide-1) medications are available on the market, offering multiple options for patients.
- Supply chain issues pose the potential for accessibility limitations.
But what can benefits leaders do to manage costs while ensuring the right patients receive these next-generation treatments?
Organizations vary in terms of the amount of access they are able to afford to these medications. Nonetheless, every organization should endeavor to ensure the right patients are receiving the right medications at the right time. The following are strategies that employers can implement to help achieve that goal, supported by the highly experienced team of experts at EPIC Pharmacy Solutions, powered by PSG.
Proactive Strategies for Plan Sponsors
- Plan sponsors can implement utilization management (UM) strategies for GLP-1 medications, considering factors like supply limits, refill thresholds, and benefits considerations for diabetes and obesity management.
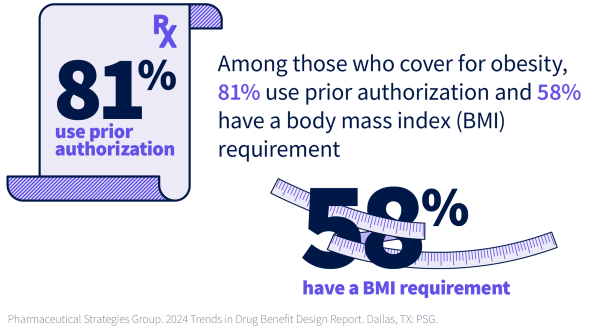
- UM criteria may involve prior authorizations, lifestyle modification programs, and stringent approval processes to ensure the appropriate use of GLP-1s.
Plan Sponsor and Pharmacy Benefit Manager Collaboration
Plan sponsors and pharmacy benefit managers (PBMs) can collaborate to develop customized utilization management programs for diabetes and obesity.
- Align on clinical criteria
Plan sponsors and PBMs should work together to define the appropriate clinical criteria for coverage of GLP-1 medications, such as diagnosis, lab values, and previous treatment history. This process ensures the right patients receive the right medications at the right dose. - Implement step therapy
Plan sponsors can work with PBMs to implement step therapy, requiring a trial of lower-cost medications before approving GLP-1s. This strategy helps manage costs while still providing access to effective treatments. - Leverage data and analytics
PBMs can provide plan sponsors with detailed data and analytics on GLP-1 utilization and outcomes. This review allows plan sponsors to identify opportunities to optimize the program and make informed decisions. - Customize prior authorization requirements
Strategic prior authorization (PA) criteria can help balance clinical appropriateness and cost control, such as requiring documentation of lifestyle modifications. - Integrate lifestyle intervention programs
Lifestyle modification programs, like nutrition counseling and fitness tracking, complement GLP-1 therapy and promote long-term health. - Monitor and adjust
Ongoing monitoring and periodic review of the utilization management program allows plan sponsors and PBMs to adjust as needed to ensure the program remains effective and aligned with the plan’s goals.
Get your copy of our GLP-1s: 2024 Trends in Drug Benefit Design Report Findings to help you make the best decisions in the current benefits landscape.
Stay Informed and Be Proactive
As the GLP-1 medication landscape evolves, stay informed about market trends, drug approvals, proactive strategies, and available support services to enhance patient care and optimize outcomes.
EPIC Pharmacy Solutions, powered by PSG, offers pre-negotiated agreements, pricing models, clinical options, and plan design flexibility to assist in optimizing GLP-1 management strategies for employers, including drivers of future growth for GLP-1s. Connect with an expert to learn more.
Download your copy of GLP-1s: 2024 Trends in Drug Benefit Design Report Findings from the form on this page to learn about your peers’ experience navigating the GLP-1 landscape.
1 Source: National Diabetes Statistics Report. Centers for Disease Control and Prevention 2024
2 Source: Adult Obesity Facts. Centers for Disease Control and Prevention 2024
EPIC offers this material for general information only. EPIC does not intend this material to be, nor may any person receiving this information construe or rely on this material as, tax or legal advice. The matters addressed in this document and any related discussions or correspondence should be reviewed and discussed with legal counsel prior to acting or relying on these materials.
Contact the Author
Sarah Fleming, PharmD, Senior Pharmacy Benefit Clinical Consultant | EPIC Pharmacy Solutions, powered by PSG | Contact Sarah via phone or email.
Related Content
Products
Employee Benefits Consulting
Our dedicated benefits team is focused on delivering better outcomes – to both your benefits program and ...
Products
Pharmacy Solutions
Our Pharmacy Consulting Practice helps companies navigate the unique complexities of expertly managing the ...
Products
Actuarial
Our Actuarial Team provides guidance on employee benefits and health and welfare programs to help meet ...